Managing type 2 diabetes can be a complex journey, and finding the right treatment that works for you is essential for maintaining good health.
One medication that has gained popularity in recent years for its effectiveness is Ozempic (semaglutide).
However, not everyone experiences the same results. If you’re wondering, “Why is Ozempic not working for me?” you’re not alone.
In this blog post, we will delve into the various factors that can influence Ozempic’s efficacy in managing diabetes.
From lifestyle choices and medication adherence to individual responses and underlying health conditions, there are several variables at play.
By understanding these factors, you can have a more informed discussion with your healthcare provider and explore alternative treatments to better control your blood sugar levels and improve your well-being.
What Is Ozempic?
Ozempic is a prescription medication used to treat type 2 diabetes. Its active ingredient, semaglutide, belongs to a class of drugs called GLP-1 receptor agonists.
Ozempic works by mimicking the action of a hormone called glucagon-like peptide-1 (GLP-1) in the body, which helps regulate blood sugar levels.
People with type 2 diabetes can use Ozempic to help lower their blood sugar levels by stimulating the release of insulin and reducing the amount of sugar produced by the liver.
It also helps slow down the absorption of sugar from the digestive system and promotes a feeling of fullness, which can aid in weight management.
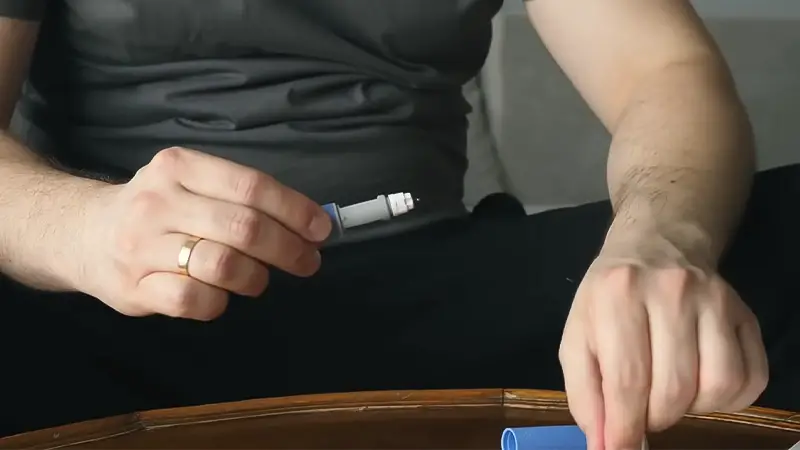
Ozempic is typically administered once a week as a subcutaneous injection. It has been found to be effective in improving blood sugar control and may be prescribed alongside other diabetes medications or as a standalone treatment.
It’s essential to use Ozempic as directed by a healthcare professional and to combine it with a healthy diet and lifestyle for optimal diabetes management.
How Does Ozempic Work on the Human Body?

Ozempic (semaglutide) works in several ways to help regulate blood sugar levels in the human body, making it a valuable treatment for type 2 diabetes:
GLP-1 Receptor Agonist
Ozempic belongs to a class of drugs called GLP-1 receptor agonists. It mimics the action of a natural hormone called glucagon-like peptide-1 (GLP-1) in the body.
Increased Insulin Release
When blood sugar levels rise after eating, Ozempic stimulates the pancreas to release more insulin into the bloodstream.
Insulin is a hormone that helps cells take up sugar (glucose) from the blood, reducing high blood sugar levels.
Reduced Liver Sugar Production
Ozempic also inhibits the liver’s production of excess glucose.
In people with type 2 diabetes, the liver can release too much glucose into the bloodstream, contributing to high blood sugar levels. Ozempic helps decrease this process.
Slower Digestion of Food
The medication slows down the emptying of the stomach, which helps to control the rate at which sugar is absorbed from food into the bloodstream.
This can help prevent rapid spikes in blood sugar levels after meals.
Appetite Control
Ozempic can reduce appetite and promote a feeling of fullness (satiety). This can aid in weight management, as it may lead to reduced food intake and, consequently, weight loss.
Long-Lasting
Ozempic is typically administered as a once-weekly subcutaneous injection, providing sustained blood sugar control over several days.
It’s important to note that Ozempic is prescribed by healthcare professionals and should be used as part of a comprehensive diabetes management plan, which often includes dietary changes and lifestyle modifications.
Why Is Ozempic Not Working For Me?
If Ozempic (semaglutide) does not seem to be effectively managing your type 2 diabetes, there could be several reasons for this:
Incorrect Usage
Ensure that you are using Ozempic as prescribed by your healthcare provider.
This includes the correct dosage, administration technique, and timing of injections. Any deviations from the recommended regimen can affect its effectiveness.
Resistance or Tolerance
In some cases, the body may develop a tolerance to GLP-1 receptor agonists like Ozempic over time.
This can result in reduced efficacy. Your healthcare provider may need to adjust your dosage or explore alternative treatment options.
Diet and Lifestyle Factors
Ozempic works best when combined with a healthy diet and regular physical activity.
If you have not made necessary dietary changes or are not engaging in regular exercise, it can limit the medication’s effectiveness.
Other Medications
Some medications can interact with Ozempic and affect its performance.
Inform your healthcare provider of all the medications you are taking, including over-the-counter drugs and supplements, to rule out potential drug interactions.
Disease Progression
Over time, the nature of diabetes can change. As the disease progresses, your body’s response to medications like Ozempic may alter. Your healthcare provider may need to reassess your treatment plan.
Individual Variations
People with type 2 diabetes can have varying responses to medications due to individual differences in physiology.
What works for one person may not work the same way for another. Your healthcare provider may need to explore different treatment options.
Underlying Health Issues
Other health conditions, such as thyroid disorders or kidney problems, can impact the effectiveness of diabetes medications. Ensure your healthcare provider is aware of your complete medical history.
Patient Compliance
Ensure you are adhering to your treatment plan consistently. Missing doses or not following dietary and lifestyle recommendations can affect the medication’s efficacy.
Reevaluation
If you have been using Ozempic for an extended period without satisfactory results, it may be necessary for your healthcare provider to reevaluate your overall diabetes management plan.
This may include considering different medications or treatment strategies.
It’s crucial to communicate openly with your healthcare provider if you feel that Ozempic is not working as expected.
What to Do If Ozemic Doesn’t Work on You?
If Ozempic (semaglutide) is not effectively managing your type 2 diabetes or if you and your healthcare provider have decided to explore alternative treatments, there are several other medications and approaches that can be considered.
Here are some basic alternatives and steps to replace Ozempic:
Alternative GLP-1 Receptor Agonists
If Ozempic isn’t delivering the desired results, your healthcare provider may consider switching you to a different GLP-1 receptor agonist medication.
Options include medications like Bydureon (exenatide extended-release) or Trulicity (dulaglutide). These drugs work in a similar way to Ozempic but may have different effects on your body.
Insulin Therapy
In some cases, individuals with type 2 diabetes may require insulin therapy. This can involve different types of insulin, such as long-acting and short-acting insulin, to help control blood sugar levels.
Your healthcare provider will determine the appropriate insulin regimen and dosage for you.
Oral Medications
There are several classes of oral medications for type 2 diabetes, including metformin, sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors, and more.
Depending on your specific needs and medical history, your healthcare provider may recommend one or more of these medications as an alternative to Ozempic.
Lifestyle Modifications
Continue to focus on a healthy diet and regular physical activity. These lifestyle changes are crucial for managing type 2 diabetes and can often complement medication.
Work with a registered dietitian or diabetes educator to create a personalized meal plan.
Regular Blood Sugar Monitoring
Regardless of the treatment option chosen, consistent monitoring of your blood sugar levels is essential.
This helps you and your healthcare provider make informed decisions about medication adjustments and lifestyle changes.
Consult with a Specialist
If Ozempic has not worked for you, it may be beneficial to consult with an endocrinologist or a diabetes specialist.
They have expertise in managing complex diabetes cases and can offer additional insights and treatment options.
Consider Combination Therapies
Your healthcare provider may recommend combining different diabetes medications to optimize blood sugar control.
Combining medications with different mechanisms of action can sometimes be more effective than using a single medication.
Patient Education and Support
Joining a diabetes support group or working with a certified diabetes educator can provide valuable information and support for managing your condition effectively.
It’s important to remember that managing type 2 diabetes often involves a trial-and-error process to find the most suitable treatment for your individual needs.
Benefits and Side Effects of Using Ozemic

It’s crucial to discuss the benefits and potential side effects of Ozempic with your healthcare provider.
Benefits of Using Ozempic (Semaglutide)
Blood Sugar Control
Ozempic is highly effective in lowering and controlling blood sugar levels in people with type 2 diabetes.
It stimulates insulin release, reduces liver sugar production, and slows the absorption of sugar from the digestive system.
Weight Loss
Many individuals using Ozempic experience weight loss as a side effect. This is due to the medication’s ability to reduce appetite and promote a feeling of fullness, leading to reduced calorie intake.
Cardiovascular Benefits
Ozempic has been associated with cardiovascular benefits, including a reduction in the risk of major cardiovascular events like heart attacks and strokes in some clinical trials.
Once-Weekly Dosing
Ozempic is administered as a once-weekly injection, making it more convenient for many people compared to daily medications.
Low Risk of Hypoglycemia
Ozempic has a low risk of causing hypoglycemia (low blood sugar) when used as a monotherapy. This makes it a safer option for people who are prone to hypoglycemia.
Common Side Effects of Ozempic
Nausea
Nausea is a common side effect, especially when starting Ozempic. It typically decreases over time as the body adjusts to the medication.
Vomiting
Some individuals may experience vomiting, particularly during the initial weeks of treatment.
Diarrhea
Diarrhea can occur as a side effect of Ozempic use. It is usually mild to moderate in severity.
Abdominal Pain
Abdominal discomfort or pain may be experienced by some users.
Decreased Appetite
While this can contribute to weight loss, it may also lead to reduced food intake, which could affect overall nutrition.
Injection Site Reactions
Redness, itching, or swelling at the injection site may occur but is usually mild and temporary.
Less Common Side Effects
Pancreatitis
Although rare, Ozempic may increase the risk of pancreatitis (inflammation of the pancreas). Seek medical attention if you experience severe abdominal pain.
Kidney Problems
Some individuals may experience changes in kidney function, so regular monitoring is essential.
Allergic Reactions
In rare cases, severe allergic reactions to Ozempic may occur, with symptoms such as rash, itching, swelling, severe dizziness, or difficulty breathing. Seek immediate medical attention if this happens.
FAQs
Why doesn’t Ozempic seem to be lowering my blood sugar effectively?
Several factors can influence Ozempic’s effectiveness, including diet, lifestyle, medication adherence, and disease progression.
If you’re concerned, consult your healthcare provider for a review of your treatment plan and potential adjustments.
Can insulin resistance affect Ozempic’s performance in managing diabetes?
Yes, insulin resistance can impact how Ozempic works.
If you have significant insulin resistance, your healthcare provider might need to explore alternative treatment options or combination therapies to achieve better blood sugar control.
What should I do if I experience side effects with Ozempic?
If you experience side effects like nausea, vomiting, or diarrhea, consult your healthcare provider. They can offer strategies to manage side effects or consider alternative medications if necessary.
Can lifestyle changes help improve Ozempic’s effectiveness?
Absolutely. Combining Ozempic with a healthy diet and regular exercise can enhance its efficacy in managing diabetes and achieving weight loss.
Discuss lifestyle modifications with your healthcare provider to create a comprehensive diabetes management plan.
How long should I give Ozempic before deciding if it’s not working for me?
It’s recommended to use Ozempic for at least 3-6 months to evaluate its effectiveness fully.
If you still don’t see the desired results or experience concerning side effects, consult your healthcare provider for a review of your treatment options.
Patience and communication with your healthcare team are key.
Wrapping Up
In the quest to manage type 2 diabetes effectively, it’s crucial to remember that there is no one-size-fits-all solution. If Ozempic isn’t delivering the desired results, it doesn’t mean you’re out of options.
By working closely with your healthcare provider, you can identify the specific reasons why Ozempic may not be working for you and develop a tailored plan that may involve alternative medications or combination therapies.
The key is patience and open communication with your healthcare team. Diabetes management is a dynamic process, and adjustments to your treatment plan may be necessary.
Your journey to better blood sugar control may involve some trial and error, but with the right guidance, you can take steps towards improved health and well-being.
Remember that your healthcare provider is your partner in this journey, and together, you can find the most suitable approach to managing your diabetes. Thank you.
Hi, I’m Mark Pattinson and I’m a freelance personal trainer. I’ve been working in the fitness industry for over 10 years especially since I work with diabetes patients and I love helping people achieve their fitness goals. I believe that everyone can benefit from a good workout, and I’ll do everything to make sure you get the most out of your training.